Hyaluronidase
The antidote
Dr Pamela Benito discusses the uptick in patients requesting to have their filler dissolved, and how hyaluronidase should be administered
Dr Pamela Benito
Dr Pamela Benito
Dr Pamela Benito is a specialist aesthetic doctor with over ten years of clinical experience and a passion for artistry in her approach. She graduated as a dental surgeon in Madrid and completed a Master’s degree in Aesthetic Dentistry at the University of New York. She switched to facial aesthetics full time tin 2015 and now consults across a number of clinics in London. Follow her on Instagram: @drpam.aesthetics
C elebrity culture has undoubtedly popularised dermal fillers, but it has also had a negative impact on how the treatment is perceived, with many people mistakenly associating fillers with an un-natural and “overly done” look.
Beauty trends are forever changing and, recently, several celebrities such as Love Island contestant Molly-Mae Hague, TV personality Gemma Collins and Kardashian sister Kylie Jenner have decided to reverse their cosmetic fillers and go back to their natural looks, openly talking about it to the media.
I suspect that many of these celebrities noticed how un-natural they were looking; that the large lips, high cheekbones and sharp jawlines that were so popular over the past few years are now going out of fashion. There are a lot of overdone faces out there and I think, thankfully, we are now moving towards a more natural look. There is now an opportunity for celebrities to still have dermal filler treatments but have them done tastefully; strategically placed and in minimal quantities to create a more youthful look.
In recent years, I have personally experienced a rise in patients requiring their dermal fillers to be dissolved, mainly due to unwanted results (asymmetry, lumps, migration, Tyndall effect and /or overcorrection). I definitely think that the increase in patients having filler dissolved is a result of not just beauty trends, but also of filler miseducation, like when “packages” of filler are sold by the ml for (overcorrection or misplacement of HA filler), or in cases of allergic reactions to the dermal filler. Also, if a patient has had filler treatment and is no longer happy with how they look or has been to a practitioner who was maybe not so adequately trained that has left them with lumps, nodules or filler migration, they may wish to dissolve the filler.
When an area is overfilled with dermal filler, it causes excess swelling and stretching of the tissue. Once the HA filler is dissolved, it can take some time for the skin to tighten back, and there may be cases where the skin doesn’t return to its original shape; in this instance, non-invasive treatments may be needed to encourage tightening and rejuvenation of the treated area.
“The increase in patients having filler dissolved is a result of not just beauty trends, but also of miseducation”
The most common area where patients have filler dissolved is definitely the lips; an area that if not treated correctly, is very obvious. Sometimes, it pre-determined areas before the patient is even consulted. We should challenge this business model of filler up-selling to ensure that people are being treated as patients rather than consumers, and that those seeking aesthetic treatments are treated by qualified medical practitioners.
Reverse effect
Bruising and swelling is common posttreatment with filler, but these effects are temporary. As with any injection, it is possible that patients may experience some redness, swelling, tenderness and bruising. These may take 24-72 hours to resolve, and bruises sometimes longer. After a few days, the treated area should return to its natural state and patients should wait at least two weeks before having any other filler treatment.
However, if the filler needs to be dissolved, hyaluronidase is used to prevent complications from inappropriate injection of HA, such as Tyndall effect, delayed onset nodules and for correcting unacceptable cosmetic outcome can simply be down to the fact that the lips are overfilled and they can look unnatural, as opposed to looking beautifully balanced and soft. Poor placement and migration can also be an issue when the lips have been treated. This can make the border of the lips look overly projected and full in an extremely un-natural way.
Another area where we often have to dissolve filler is the tear trough; the skin around this area is delicate and thin so if it has been overtreated with filler it will be easily visible. 7 Sometimes, this can result in an uneven or lumpy appearance, or in some cases, Tyndall effect can be visible. This can worsen the appearance of dark circles under the eye. Both can be due to poor filler choice, placement, a lack of anatomy knowledge, or these factors combined.
Hyaluronidase 101
Different HA fillers have differing physical properties that influence their degradation by hyaluronidase in a time and dosedependent manner. 2 Hyaluronidase may be reconstituted with either saline or water for injection. Saline is less painful on injection and is recommended for this reason. Although unlicensed for this purpose, bacteriostatic saline is often preferred for its additional anaesthetic properties.
The volume of diluent used will depend on the indication and surface area to be treated. A range of 1-10mls has been evidenced in clinical practice and published papers.
According to the ACE Group, before proceeding to treat with hyaluronidase it is safe and expected practice that a patch test should always be performed, except when the indication is for vascular compromise and a delay could result in further harm to the patient. An intradermal injection of 3-4 IU of hyaluronidase in the forearm has been advocated after observing the results after 30 minutes.
Prior to injection, the area should be inspected, palpated and marked out if needed. It should then be cleansed and disinfected using an appropriate skin solution and the procedure should be carried out using an aseptic technique. A 30G needle with an appropriate length to treat the depth of the area should be used. Administration should be accurate and limited to the affected area. 2 For vascular compromise, serial puncture should be used to inject hyaluronidase along the course of the vessel and covering the affected area. During and after the procedure, the treated area should be massaged rather vigorously to optimise the result and aid mechanical breakdown.
The most difficult part of using hyaluronidase is estimating the dosage amount required to dissolve the filler. A consensus opinion in the literature states five units of hyaluronidase is needed to break down 0.1ml of 20mg/ ml HA, although there is quite a range. It is recommended to inject as much hyaluronidase as required to obtain the desired effect rather than following an absolute dosage. 6 As dissolving filler is “off-label”, there is no manufacturer guidance on how much to use for this purpose. The required amount depends on the filler characteristics, volume, and distribution.
Although the amount injected should be titrated to clinical effect, Table 1 offers a guide to actual dosages used in published articles.
Hyaluronidase has immediate effect and a half-life of two minutes with duration of action of 24 to 48 hours. 4 Though it has a short half-life, its effectiveness lasts longer.
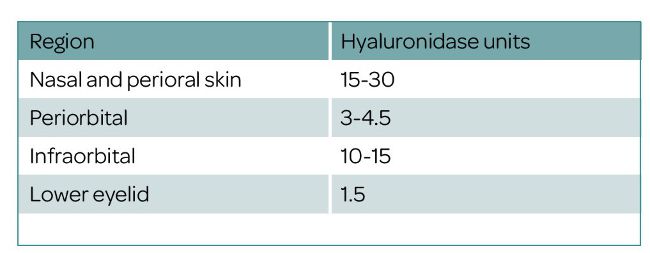
Table 1: Aesthetic Complications (ACE) Group UK guidelines on hyaluronidase units per region 4
This might be due to the low number of units required to have a clinically significant effect; thus, even when the hyaluronidase has mostly degraded, its action continues.
Additionally, hyaluronidase may degrade the body’s natural HA in preference to foreign HA filler that has been injected and specifically cross-linked to prevent its natural breakdown. So, the initial action of hyaluronidase might break cross-links in the HA dermal filler so that it behaves like native HA in the skin, which has a half-life of 24 to 48 hours.
Hyaluronidase is also used off-label in chronic pain management to facilitate removal of epidural adhesions and to treat oedema. 5
Finer details
The more cross-linked a gel is, the longer it can last in the body and the more it will resist breakdown by both native and injected hyaluronidase. This is why certain fillers with higher viscosity and crosslinking may require multiple hyaluronidase injections to dissolve. Also, it has been found that some patients taking high doses of aspirin, cortisone, oestrogen, and antihistamines may have tissue that is more resistant to the spreading effect of hyaluronidase.
I would recommend re-treatment no earlier than two weeks to avoid breakdown of any consecutive HA filler and to allow for any bruising and swelling to have completely resolved, and the patient is back to baseline.
There are non-dissolvable fillers on the market like hydroxylapatite (Radiesse), poly-l-lactic acid (Sculptra), polymethyl methacrylate (Bellafill), and off-label liquid silicone (Silkon-1000) which are not reversible or dissolvable with hyaluronidase. However, these, along with bio-stimulating fillers, are not as commonly used as HA fillers.
Allergic reactions are a side effect of hyaluronidase. While allergy in the injection area is very rare, it can be severe and may include the risk of anaphylaxis. The incidence of allergic reactions is reported to be 0.05% to 0.69%, and urticaria and angioedema have also been reported to occur at a low frequency (less than 0.1%). Allergic reactions are more likely to occur when the dose is more than 100,000 IU through an intravenous injection. 5 Most allergic reactions are immediate hypersensitivity reactions and manifest as erythematous oedema after one to two hours, and there is no response to antibiotic therapy. In such cases, systemic steroids and antihistamines are helpful.
Since most allergic responses to hyaluronidase are immediate hypersensitivity reactions, skin tests are recommended before use. However, some patients experience delayed allergic reactions, which skin tests may not predict. There is usually no link between a history of allergies and the response to hyaluronidase. However, depending on the origin of the hyaluronidase, its injection should be avoided in patients who are allergic to bee stings and bovine collagen. 1 Delayed hypersensitivity reactions can occur even after 24 hours, and in such cases, a skin patch test will not produce a positive reaction within 20 minutes, resulting in a negative diagnosis.
Bruising and swelling after hyaluronidase treatment are common. Patients may also experience pain, itching or redness where the injection has been given.
As previously mentioned, hyaluronidase does likely degrade native hyaluronic acid found in skin and subcutaneous tissue, but long-term deficiency has not been described in the literature and the continual production of hyaluronic acid should lead to a restoration within days.
It has been reported, but without significant corresponding evidence in the literature, that repeated injections of large amounts of hyaluronidase could result in the formation of neutralising antibodies that would render hyaluronidase less effective. The only case studies describing complications are related to hypersensitivity reactions but did not uncover any reports of iatrogenic skin or soft-tissue injury attributed to hyaluronidase.
Hot topic
There is an exciting recent development in the area of hyaluronidase and filler dissolving. SoftFil Topilase is a topical treatment that safely shapes and reduces the unwanted presence of hyaluronic acid to adjust the skin’s ideal hyaluronic acid level.
This truly innovative cosmetic has a unique formulation which provides a noninvasive response to excess hyaluronic acid and restores the skin surface by reducing the appearance of irregularities and defects linked to HA-filler injection. However, despite being topical, Topilase is still intended for use by a healthcare professional only after a skin diagnosis.
Hyaluronidase use has become more diverse and widespread in clinical practice. In particular, it is used to address patients’ dissatisfaction after hyaluronic acid filler treatment and to treat side effects. As its use becomes more common, it is increasingly important for clinicians to have a sufficient knowledge of hyaluronidase. It can serve as an appropriate treatment in a variety of situations if it is used with a thorough understanding of its mechanism of action, metabolism, and side effects. It is a prescription-only medicine and the potential side-effects and risks can be significant. Therefore, it is important that patients see a medical practitioner for filler-dissolving treatments.
REFERENCES
1. Hyaluronidase: An Overview of its properties, applications, and side effects. Arch Plast Surg. 2020 Jul: 47(4): 297-300.
2. The Use of Hyaluronidase in Aesthetic Practice. J Clin Dermatol. 2018 June: 11(6): E61-E68.
3. M Dalvi Humzah, Saj Ataullah, ChenAn Chiang, Raman Malhotra, Robert Goldberg. The Treatment of Hyaluronic Acid Aesthetic Interventional Induced Visual Loss (AIIVL): A Consensus on Practical Guidance. J Cosmet Dermatol. 2019 Feb;18(1):71-76.
4. Martyn King, MD; Cormac Convery, MD; and Emma Davies, RN. The Use of Hyaluronidase in Aesthetic Practice Journal of Clinical and Aesthetic Dermatology 11(6):E61-E68
5. Maurizio Cavallini, Riccardo Gazzola, Marco Metalla, Luca Vaienti, The Role of Hyaluronidase in the Treatment of Complications From Hyaluronic Acid Dermal Fillers, Aesthetic Surgery Journal, Volume 33, Issue 8, November 2013, Pages 1167–1174.
6. ACE Group, The Use of Hyaluronidase in Aesthetic Practice, February 2014.
7. Bailey S, Cohen J et al., Etiology, Prevention and Treatment of Dermal Filler Complications, Aesthetic Surgery Journal, January 2011.