GROWTH FACTOR CONCENTRATE
Treating pigmentary disorders
Dr Madhuri Agarwal elaborates on autologous growth factor concentrate (GFC) highlighting its protocols and procedure along with factors that make it better than PRP.
Dr Madhuri Agarwal

Picture: For representational purpose
Pigmentary disorders typically indicate an increased amount of melanin, leading to darker colour of the skin, called hypermelanosis or hyperpigmentation. It has been seen in various studies that skin hyperpigmentation has considerable psychological impact on an individual and leads to impaired quality of life.
Common types of hyperpigmentation disorders
Melasma: This is predominantly seen on sun-exposed areas of the face in women and exposure to sunlight, cosmetics, pregnancy, hormonal treatments, thyroid dysfunction, phototoxic drugs, and anticonvulsant medications and genetics have been implicated in the pathogenesis of melasma.
Periorbital melanosis: Dark circles under the eyes are common and can occur due to exhaustion, lack of sleep, allergies, eye rubbing or excessive sun exposure, family history of dark circles, or any other hyperpigmentation disorder.
PIH (Post-inflammatory Hyperpigmentation): Any inflammatory condition in the skin (fr instance, eczema, psoriasis, and acne scars), especially in dark-skinned patients, can lead to post-inflammatory hyperpigmentation, characterised by patches of brown skin.
Diffuse hyperpigmentation (DHP): Is usually due to systemic cause, such as Addison’s disease, hyperthyroidism, or hemochromatosis. It also may occur because of a certain medication side-effect.
Acanthosis nigricans: Typically occurs in people who are obese or have diabetes. More rarely, it can be a warning sign of a cancerous tumour in an internal organ, such as the stomach or liver. Dark, velvety patches of skin often appear in the armpits, groin and neck.
Lichen planus pigmentosus (LPP): This is an inflammatory skin disorder, oval or irregularly-shaped brown to graybrown coloured patches commonly on sun exposed area such as the forehead, temples and neck. The condition may be triggered by viral infections, UV light or the application of certain oils to the hair or skin (such as mustard oil, amla oil, or henna hair dyes).
Erythema dyschromicum perstans (EDP): Also called ashy dermatosis, is a rare acquired and chronic dermatosis, characterised by asymptomatically and progressively hyperpigmented macules of various size on the trunk, face, and extremities.
LIMITATIONS OF CURRENT THERAPIES IN PIGMENTARY DISORDERS
The current anti-pigmenting agents can inhibit melanogenesis partially and the results are often unsatisfactory. The treatment with anti-pigmenting agents has to be continued for several months before any clinical benefits are seen. Topical agents used for hyperpigmented skin area are potent anti-melanogenic agents and are capable of suppressing constitutive pigmentation. This may lead to hypo pigmentation in surrounding areas. A relapse and rebound of condition is not uncommon after stoppage of antipigmenting treatment. Hence, inhibition melanogenesis in a controlled manner with sustained benefit would be an appropriate approach for a new development of new therapy.
WHAT IS PRP?
The platelet-rich plasma (PRP), plasma with concentrated platelets is a relatively old technique, which is used in many branches of medicine. It is an effective concentration of multiple fundamental growth factors (GFs) by virtue of platelets alone (stored as -granules in platelets) and plasma proteins, namely fibrin, fibronectin and vitronection. The cocktail of GFs is pivotal in modulation of tissue repair and regeneration, whereas the plasma proteins act as a scaffold for the bone, connective tissue and epithelial migration. PRP by virtue of its autologous in nature, minimal chances of side-effects and its action through concentrated growth factors, has become popular in the last two decades in aesthetic dermatology. Studies have highlighted the potential benefit of PRP in the treatment of hyperpigmentation.
MECHANISM OF PRP ACTION IN PIGMENTARY DISORDERS
Platelets contain a-granules, which have greater than 30 bioactive substances in it such as platelet-derived growth factor (PDGF), epidermal growth factor (EGF) and transforming growth factor (TGF)-b1 and TGF-b2, which are released after PRP injection. It has been found that TGF-b1 inhibits melanin synthesis in a concentration-dependent manner through delayed extracellular signal-regulated kinase activation. EGF lowers melanin production in melanocytes by inhibiting prostaglandin E2 (PGE2) expression and tyrosinase enzyme activity. Other growth factors such as PDGF, VEGF improves skin volume (blood vessel formation, collagen synthesis, and extracellular matrix formation) promoting skin regeneration and rejuvenation.
LIMITATIONS OF PRP
• Variable platelet output: Although platelets are collected in high concentration, there is a loss of variable number of platelets during the procedure.
• Unknown and suboptimal concentration of growth factors: Platelets obtained from most of the PRP are in inactivated form and require activation to release GFs, it is still a matter of further research that:
• -How exactly platelets are activated? -How many platelets are activated? -How many Growth factors are released?
• Risk of contamination
• Risk of inflammation and pain
• Needs to be used immediately
What is autologous growth factor concentrate (AGFC)?
AGFC or simply GFC is an innovative technology developed by Wockhardt, where the patient’s blood is processed, so as the final outcome has a high concentration of growth factor released after platelet activation. Growth output is consistent without any unwanted cells reducing the chances of pain and inflammation. It contains specific growth factors at high concentration. These growth factors include: - Transforming growth factor beta (TGF- ) - Epidermal growth factor (EGF) - Platelet-derived growth factor (PDGF) - Vascular endothelial growth factor (VEGF) - Fibroblast growth factor-2 (FGF-2)
Protocols of AGFC
• Three sessions are done at an interval of a month.
• Pre-treatment photography, after a month, end of third session and after every three months to monitor the longevity of results.
• Monotherapy with AGFC in melasma and skin rejuvenation. All skin lightening and antiaging topical as well as other procedural treatments are stopped three months before therapy.
• AGFC is combined with microneedling RF (MNRF) in acne scars or can be done solely.
• Patients were advised to use sunscreen and moisturising creams for the duration of treatment.
Procedure of AGFC
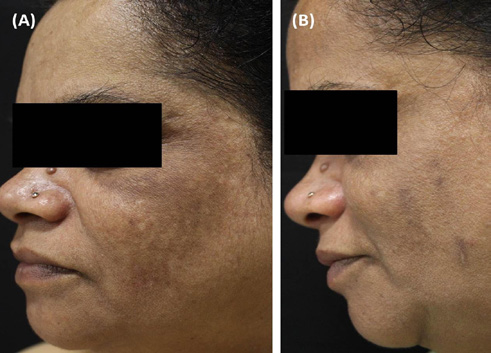
Skin appearance of 50-year-old female (A) before the Yuskin GFC therapy at Day 0 (mMASI score:14.1) and (B) one month after the three sessions of Yuskin GFC therapy at Day 90 (mMASI score:7.4)
Clinical evidence
Sthalekar and Madhuri Agarwal et al. (July 2021) in Melasma patients has demonstrated a significant reduction in melasma score with Yuskin GFC therapy as a monotherapy. Statistically significant decrease in the mean melasma scores was observed at early as one month just after one session and improvement was continued even one month after the last session. Overall, aesthetic improvement was noted in 88.5 per cent of subjects at the end of the study by both doctors and patients themselves. Improvement from baseline was noticeable as early as day Recently, a study conducted by Bindu 30 with one GFC session in 55.9 per cent of subject. Overall, GFC therapy was well tolerated and found to be a safe, effective and a new option in reducing the hyperpigmentation.
How GFC therapy is better than PRP?
In conclusion
• Pigmentary disorders are challenging and difficult to treat.
• In procedures aiming at aesthetic improvement, patient perception of the treatment outcome appears to be most important because it has a direct impact on the patient’s body image and self-esteem.
• Autologous growth factor concentrate patent is a unique, innovative treatment, as it treats pigmentary disorders with long term remission.
• Unlike PRP, there is a consistent release of growth factors with negligible downtime and adverse effects.
• AGFC gives a uniform reproducible result in skin.
• Furthermore, many patients have mentioned about experiencing a remarkable improvement in skin quality in addition to a more stable and balanced skin colour and subsequently can wear more natural makeup.

Picture: For representational purpose
Dr Madhuri Agarwal
With over 15 years of experience, Dr Madhuri Agarwal is the Founder and Medical Director of Yavana Aesthetics Clinic. She regularly travels across the globe to enrich herself with the best practices and state-of-the-art technology to bring it to the Indian aesthetic aspirants. She gets invited regularly to deliver talks on cosmetic treatments nationally and internationally to her peers and to the public. From the past few years, she has been actively involved in training other fellow dermatologists and aspirants, the art and techniques of laser, facial rejuvenation, anti-ageing and dermal fillers.