Treatment modalities for acne scars
Acne and acne scars affect more than just adolescents. Dr Sejal K Shah shares in-depth information on the types and the numerous treatments that are available for acne scars.
Acne is a common inflammatory disorder of the pilo-sebaceous units, affecting most adolescents; and it can continue as adult acne as well. Scarring is a sequela of any grade of acne and can have a marked impact on one’s quality of life. Genetic factors, disease severity and delay in treatment can influence scar formation(1,2).
CLASSIFICATION OF ACNE SCARS
There are two basic types of acne scars depending on whether there is depletion (atrophic) or net gain of collagen (hypertrophic) during the healing of acne.(2,3)
This classification is keeping in mind the therapeutic options. Atrophic scars (80-90 per cent of all acne scars) are further divided into ice pick scars (60-70 per cent of all), boxcar scars (20-30 per cent), and rolling scars (15-25 per cent).(3,4,5)
These scars can in turn be erythematous, hyperpigmented or hypopigmented.
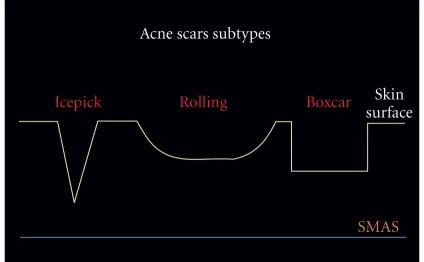
Acne scar subtypes [2]
Hypertrophic and keloidal acne scars form due to excessive collagen deposition.
TREATMENT MODALITIES
There are several modalities available for the treatment of acne scars, predominantly atrophic scars. Although there is no ‘gold standard’ modality, a combination of different technologies can be used sequentially or rotationally to give better outcomes.
The procedural treatments can be broadly divided into energy device based and non-energy device based.
The energy device-based technologies include:
• Ablative lasers
• Non ablative lasers
• Fractional radiofrequency (MNRF)
• Intense pulse light
• Plasma skin regeneration
The non-energy device-based modalities include:
• Chemical peels
• Microneedling
• Subcision
• Punch techniques
• Platelet rich plasma therapy
• Dermal fillers
• Autologous fat transfer
• Botulinum toxin
• Microdermabrasion/dermabrasion
NON-ENERGY DEVICE-BASED TREATMENTS
Chemical Peels: Chemical peels work best for macular pigmented acne scars and also for superficial atrophic acne scars by reducing post acne erythema and lightening pigmentation at the base of scars. They also help by their action on collagen remodeling and stimulation of new collagen activity and hence improve the depth and contour of the scar, and produce a softening of the scars(3,5,6). The commonly used peels are Salicylic acid 20-30 per cent, Glycolic acid 30-70 per cent, Mandelic acid 30-45 per cent, Retinol based peel 5 per cent, TCA peel 15-25 per cent, Jessner’s solution; alone or in combination(2,3,5,6). Moderate improvement has been seen in ice pick, boxcar and rolling scars with 10 per cent mandelic acid and 20 per cent salicylic acid combination peel with lesser adverse effects(7). Priming with keratolytic and lightening agents yield better outcomes with fewer side effects. On an average, around four to six sessions at an interval of two to four weeks should be done depending on the type of skin, severity of scars and the peel chosen. Medium depth peels like 25-50 per cent TCA, 40-60 per cent pyruvic acid, Jessner’s solution with 35 per cent TCA and deep peels should be used with caution, especially in colored skin.
Based on the morphology of the atrophic acne scars, these modalities can be used either alone or preferably in combination – sequentially or in rotation.(2,3,5,10)
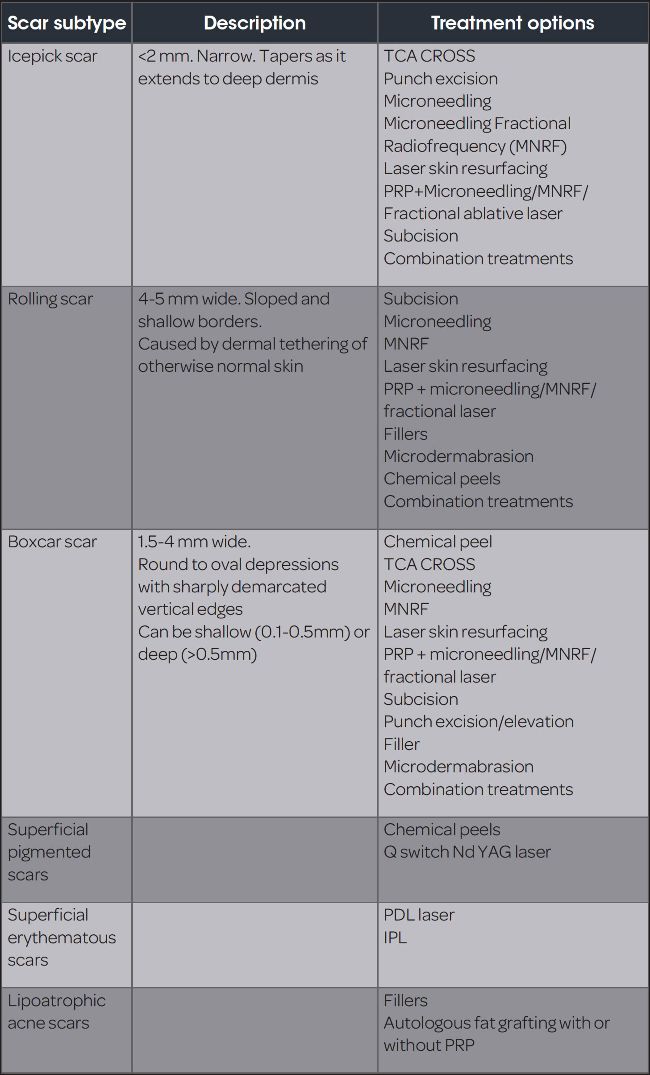
TCA Cross: TCA-chemical reconstruction of skin scars (CROSS) involves the local application of high concentration TCA with a wooden applicator to the base of the scar (2,3,5,8,9). TCA is applied for a few seconds until the scar displays a white frosting. A black crust forms in three to four days and heals in seven to ten days. The clinical effects of TCA are due to dermal collagen remodeling and an increase in the content of collagen, glycosaminoglycan, and elastin. Varying concentrations of TCA ranging from 35 per cent to 100 per cent have been used. Good to excellent improvement has been reported depending on types and grades of scars (2,8,9). Around three sittings at an interval of four weeks can be done. There is some risk of post inflammatory pigmentation, but incidence of scarring and hypopigmentation are relatively lesser (2,8,9).
Microneedling: This is a minimally invasive procedure involving superficial, controlled puncturing of the skin with miniature fine needles, either as a dermaroller or a microneedle pen. Micropunctures created by these microneedles produce a controlled skin injury without damaging the epidermis, which in turn releases growth factors and promotes neovascularization and neocollagenosis(11). The dermaroller is rolled on the stretched skin surface till there is erythema or pinpoint bleeding. Microneedle pen is an electronic microneedling device with a detachable tip with 12 fine needles, which work at varying depths in the skin depending on the setting. Four to six sessions at an interval of four to six weeks gives an appreciable result in all types of acne scars, mainly rolling and superficial boxcar scars (3,11).
Subcision: Subcision or subcutaneous incisionless surgery is a procedure in which a needle is inserted under the skin and passed in multiple directions to break the tethering fibrous bands and lift the depressed scar. A nokor needle or a simple 18G/20G or 24G (13) needle can be used. The mechanisms of scar improvement are releasing fibrotic strands underlying scars, organisation of blood in the induced dermal pocket, and connective tissue formation in the area (12,14). Rolling scars respond the best to subscision; icepick and boxcar scars show lesser response (14).
Punch techniques: Punch techniques are useful for deep depressed acne scars with sharp vertical walls such as ice pick and boxcar scars (15). These include punch elevation, punch excision, or punch grafting. In punch excision, the scar is excised and sutured along the relaxed skin tension lines, thus replacing a wide circular scar with a smaller linear scar (5,15). In punch grafting, the scar is excised and replaced by dermis from autologous donor tissue. In punch elevation or punch flotation, the depressed scar is lifted from its bed by breaking the adhesions, which bind down the scar. It is preferable to combine these techniques with subcision in a preceding session or the same session and follow up punch exicision with laser resurfacing for better results.
Platelet Rich Plasma Therapy (PRP): PRP contains high concentration of platelets, which in turn release numerous growth factors, cytokines, chemokines from alpha granules. All of these stimulate physiological wound healing and reparative tissue processes, and this helps correction of atrophic acne scars. PRP has mostly been studied as an adjuvant therapy two other treatment modalities like microneedling and fractional ablative laser. In the study by Gulanikar et al, efficacy of PRP as single modality of treatment for acne scars was evaluated. All the types of scars showed response in terms of reduction in size. Rolling scars responded better to PRP as compared to boxcar and ice pick scars(17). Studies of PRP with microneedling in atrophic acne scars have shown excellent response in boxcar, rolling scars and linear tunnel type scars with only mild and transient side-effects (16,18). Improvement in acne scars was greater when PRP was combined with fractional carbon dioxide laser (19,20). PRP also adds to the improvement in acne scars when used along with subcision and needling(21). Modarressi reported that combining fat with PRP improved fat graft survival(22).
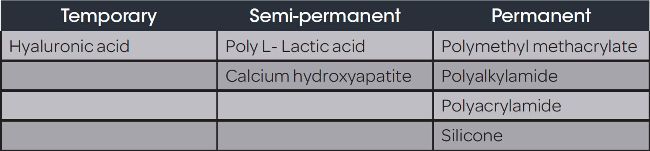
Fillers: Dermal fillers are used regularly for soft tissue augmentation, but their use in treatment of atrophic acne scars is not much documented. Fillers work by increasing tissue volume in the acne scars and inducing collagen. Fillers can be considered for boxcar and rolling scars, but deeper icepick scars do not show a good response. They can be injected by various techniques like linear threading, fanning, bolus, layering or vertical tower to enhance volume in the depressed atrophic acne scars. As of now, polymethyl methacrylate (PMMA) is the only filler approved by the US FDA for use in facial distensible atrophic acne scars.
Hyaluronic acid (HA) fillers are currently the most used fillers in soft tissue augmentation. They have been used in facial atrophic acne scars, mainly boxcar and deep rolling scars with immediate improvement. The effect lasts 6-12 months depending on the HA filler used and the technique of injection (23,24,25). Fillers can be combined with other treatment modalities like subcision, microneedling and skin resurfacing lasers for better outcomes.
Autologous fat transfer: Resolution of nodulocystic acne leaves behind wide, depressed scars, mainly in the lower face and mandibular area, known as lipoatrophic scars. These are best treated by filling with fillers or autologous fat. Fat not only helps augment the loss tissue in the scar, but also provides adipose derived stem cells which help collagen regeneration. Earlier, macrofat and microfat used to be injected in the depressed areas, but now fat is broken down to finer components to form nanofat, which is injected just below the dermis to replace lost volume and give a smooth surface. Subcision should be done before fat transfer to release tethering in order to prevent irregularities and prevent protrusion of fat. Various studies have shown efficacy of autologous fat transfer in treatment of acne scars along with preceding use of subcision or skin resurfacing laser or microneedling.(26,27)
Botulinum toxin: The use of botulinum toxin in aesthetic and certain non-aesthetic indications is well-known. Botulinum toxin has been shown to play a role in the prophylaxis and treatment of scars. It may be used to eliminate the tension produced by muscular forces surrounding the scar. There also appears to be an inhibitory effect of botulinum toxin itself on fibroblasts (28). For existing traumatic or post acne scarring, it has a role in treating scars that happen to lie in an area where they are exaggerated by movement and there will be no untoward cosmetic effect on the patient. Scarring in the upper face (forehead, periorbital, glabella) and the lower face (chin and surrounding areas) tends to be well-targeted by botulinum toxin either alone or more usually in conjunction with other techniques such as fillers, laser skin resurfacing and surgery (29).
Dermabrasion/microdermabrasion: Dermabrasion and microdermabrasion are facial resurfacing techniques that mechanically ablate damaged skin to promote re-epithelialisation. Dermabrasion completely removes the epidermis and penetrates to the level of the papillary or reticular dermis, inducing remodeling of the skin’s structural proteins. It is performed under local or general anaesthesia using a wire brush or a diamond fraise or a sterilised sand paper. Infections, persistent dyschromia, hypo- or hyperpigmentation, erythema, and scarring are possible complications. Dermabrasion is particularly successful in treating superficial atrophic acne scars, such as rolling or shallow boxcar scars (30). Strict sun protection is essential for the prevention of PIH, particularly in darker skin types.
Microdermabrasion, a more superficial variation of dermabrasion, only removes the outer layer of the epidermis, accelerating the natural process of exfoliation. The handpiece uses aluminium oxide or sodium bicarbonate crystals for abrasion, but lately a diamond tip is used for better accuracy and lesser side-effects. Microdermabrasion can be repeated at short intervals, is painless, does not require anesthesia and is associated with less severe and rare complications, but it also has a lesser effect and does not treat deep scars (31).
ENERGY DEVICE BASED TREATMENTS
Lasers and light sources: Lasers are a popular treatment option for atrophic acne scars. Lasers can be divided into:
YAG- Yttrium aluminum garnet; KTP- Potassium titanyl phosphate; IPL- Intense pulse light; YSGG- Yttrium scandium gallium garnet
- Ablative non-fractional lasers: Ablative lasers can stimulate profound dermal remodeling but require significant downtime and the associated side-effects include persistent erythema, edema, oozing, and crusting after treatment(32). Although ablative CO2 laser treatment was the gold standard for atrophic acne scars, its use is limited in dark skinned patients due to adverse effects, predominantly, post inflammatory hyperpigmentation (PIH) (33).
- Fractional lasers: These lasers work on the principle of fractional photothermolysis, a concept introduced by Manstein et al(34). This refers to the creation of pixilated columnar zones of thermal injury (microthermal treatment zones, MTZ), which are delivered to the dermis thereby stimulating collagen production and reducing healing downtime.
- Ablative fractional lasers: The commonly used fractional ablative lasers are the fractional CO2 and the fractional Erbium YAG lasers. The overall efficacy of ablative fractional lasers is higher than non-ablative fractional lasers with fewer treatment sessions needed in the former (35). Ablative fractional resurfacing with CO2 laser is evidenced based for resurfacing atrophic acne scars of moderate-to-severe variety. On the basis of various studies, it was found that ablative fractional resurfacing improved the depth and appearance of acne scars by as much as 50 per cent after a series of four to five treatments performed once a month and good textural improvement. A high-fluence, low-density setting has been shown to be more efficacious than a low-fluence, high-density setting (36,37). Most studies have shown a good response to fractional CO2 in rolling scars, though the response may be better with preceding subcision (38).
Genetic factors, disease severity and delay in treatment can influence scar formation.
- Fractional Er:YAG (2940nm): This is another fractional ablative laser used for acne scars. It produces one-third of the coagulation depth as compared to fractional CO2 laser while giving similar clinical results and lesser pain and PIH in comparison to fractional CO2 laser (39). Better results were seen in rolling and superficial boxcar scars than ice pick or deep boxcar scars(40).
- Non-ablative fractional lasers: These are the fractional 1540nm Er:glass and the 1550nm Erb-doped laser. Non-ablative fractional lasers (NAFL) use the mid-infrared wavelengths (1550, 1440, and 1927 nm) emitted by laser sources such as Er and thulium to create microscopic thermal zones (MTZ) at 200–500 µm depths. The infrared and visible wavelength ranges emitted by them stimulate the formation of Type 1 and Type 3 collagen fibers. The main benefit is the low incidence of Side-effects and faster recovery time. However, multiple sessions are needed and only a modest response is seen in severe acne scarring (38,41). Improvement in acne scarring for NAFL ranges from 25 per cent to 75 per cent in several studies, and some patients show greater than 75 per cent improvement. In a study by Sardana et al, boxcar and rolling scars responded better than icepick scars to six treatments with 1540nm non ablative fractional laser (38). The 1,550-nm erbium-doped fiber fractional laser has also been shown to be safe and effective in treating acne scarring with multiple sessions in Fitzpatrick skin Type IV to VI, though some patients have developed self-limiting post inflammatory hyperpigmentation (43,44).
- Non-ablative non-fractional lasers: These lasers deliver energy into the dermis without destroying the overlying epidermis resulting in less side effects and shorter recovery times, though the clinical improvement may be moderate, especially for deeper icepick and boxcar scars, and patients may require multiple treatment sessions(45). 1064nm Q switched Nd YAG laser- The 1,064-nm Nd:YAG laser is used for acne scarring and has shown to produce a 20 per cent to 50 per cent improvement in these lesions(46). Pulse dye laser -PDL therapy improves erythema in scars by targeting oxyhemoglobin within vascular structures in the skin, and requires three to four or more sessions at one-month intervals (47).
- Intense pulsed light: Intense pulsed light (IPL) has been used mainly to treat acne scar-associated erythema.
- Newer laser technologies: PICOSECOND 755nm ALEXANDRITE LASER
Acne scarring treated with a 755 nm picosecond alexandrite laser with a diffractive lens (DLA) is an effective treatment. In a study by Zhang et al, 29 patients received three sessions four to six weeks apart and followed up for two months. The picosecond alexandrite laser is shown in the study as an alternative in treating acne scars, and a safe and effective modality to also treat fresh scars(48).
- Radiofequency (RF) devices: RF devices use electromagnetic radiation to generate an electric current that heats the dermis causing neocollagenesis and skin contraction. Radiofrequency has decreased downtime and risk of scarring and infection compared with ablative lasers, and it is safe to use in all skin types as it is chromophore-independent, unlike other energy based modalities, such as CO2 laser.
- Microneedle Radiofrequency fractional: MNRF device works by creating radiofrequency thermal zones without epidermal injury. After damage to the reticular dermis, long-term dermal remodeling, neoelastogenesis, and neocollagenesis results in dermal thickening. The needle penetration also stimulates the release of growth factors with relative sparing of epidermis and adnexal structures, which contributes to rapid healing. MNRF has been found to be effective in reducing both atrophic acne scars and open pores. It creates a pyramidal injury zone unlike the conical thermal damage induced by ablative lasers and greater depth of penetration of the microneedles (up to 3.5 mm) as compared to fractional lasers (0.7 mm). Insulated microneedle coagulates only the deeper part and protects the epidermis, but it is associated with bleeding. Uninsulated microneedle causes coagulation along the full length of the needle, thus prevents microbleeding (49) MNRF usually requires four to six sessions for optimal results, four to six weeks apart. The majority of patients show mild to moderate (25–50 per cent) improvement (50). MNRF has minimal adverse effects such as pain, erythema, edema, and spot bleeding. Pain is significantly lower as compared to ablative fractional lasers. It is safe and moderately effective in all types of acne scars in type III and V skin (a color-blind procedure).
A combination of different technologies can be used sequentially or rotationally to give better outcomes.
COMBINATION AND MULTIMODAL TREATMENT APPROACH
Complete resolution of acne scars is a challenge even with the multiple modalities available. Combining different treatments sequentially or rotationally can give better outcomes. The goal remains to effectively exploit different technologies and treatment modalities to tackle post-inflammatory erythema, pigmentation, different types and depths of scars as well as reduce treatment downtime. Many studies have been conducted combining non-ablative lasers with ablative lasers, subcision, TCA CROSS, and PRP, to achieve better results (1,2,3,5). Subcision has been combined with fractional lasers and microneedling to take care of deeper scars. PRP has been used widely with many other modalities for better remodeling of scars and reducing post-procedure inflammation. Dermal fillers and autologous fat transplantation can be effectively combined with resurfacing procedures such as lasers or microneedling to achieve both volume restoration and rejuvenation.
NEW AND EXPERIMENTAL TREATMENTS
Autologous Non-cultured dermal cell suspension: In atrophic acne scars, the dermis is lost due to inflammation, therefore dermal suspensions could be an ideal volume replacement(3). Sahoo et al. prepared an autologous non-cultured dermal cell suspension by incubating a de-epithelialized dermal biopsy with collagenase 1. The suspension was then injected to correct localised facial volume loss. This resulted in significant improvement in the dermal atrophy group, but not in the lipoatrophy group(51).
Autologous Fibroblast Culture: Cultured fibroblasts also have been used in a pilot study by Munavalli et al (3). They treated 99 patients with injections of autologous cultured fibroblasts into acne scars(52). This was prepared by culturing skin biopsies for fibroblasts for several weeks. This was associated with significantly higher treatment success than the vehicle. There were no permanent side-effects. There was an increasing trend of improvement at four months of follow-up.
i. Jet Volumetric Remodeling:
Jet Volumetric Remodeling (JVR) is a needle-free proprietary technology, which accurately delivers kinetic energy and a healing compound at a high speed simultaneously via a tiny entry point in the epidermis. The particles, acting as nano-bullets, disperse in the dermis to create a micro trauma, which promotes neocollagenosis(3). The JVR device using HA has been used to treat acne scars in two patients in two sessions showing some improvement. There was minimal downtime(53).
The procedural treatments can be broadly divided into energy device based and non-energy device based.
ii. Radiofrequency subcision:
This modification of subcision uses radiofrequency energy for subcision(3). This method decreases the chances of postoperative bleeding and hematoma formation. The fibrotic strands get cut with ease without any mechanical force(54).
For references, CLICK HERE
DR SEJAL K SHAH,
MD (Skin & VD); DVD; DDV; MBBS, has been practising clinical and aesthetic dermatology for 20 years. She is the Medical Director at Visage Skin Clinic (Juhu, Mumbai) and Former Head Medical Advisor of Kaya Skin Clinic-India, West region. She is also a trainer for botulinum toxin and fillers, with a special interest in aesthetic dermatology and regenerative medicine.