ULTRASOUND AND INJECTABLES
METABOLIC SYNDROME and the skin
In the first of this two-part special, Balsam Alabassi explains what metabolic syndrome is and why it occurs

W eall know that our skin is the largest living organ body and often a powerful indicator of what lies beneath. It is therefore of no surprise to learn that the skin is a reflection of our internal state of health, one of which is metabolic syndrome. Metabolic syndrome was discovered by GM Reaven in 1988 and known as ‘syndrome X’.1It is defined as a collection of risk factors that are of metabolic origin and associated with an elevated risk of cardiovascular disease and type II diabetes mellitus, comprising of visceral/central obesity, atherogenic dyslipidaemia, increased blood pressure and elevated plasma glucose. 2The World Health Organization (WHO) produced the first formalised definition of the metabolic syndrome in 1998. This included impaired glucose tolerance (IGT), impaired fasting glucose (IFG) or diabetes mellitus, and/ or insulin resistance (as measured using a hyperinsulinemic euglycemic clamp study), together with two or more additional components. These components included hypertension, raised plasma triglycerides, low HDL-C central obesity and microalbuminuria.3
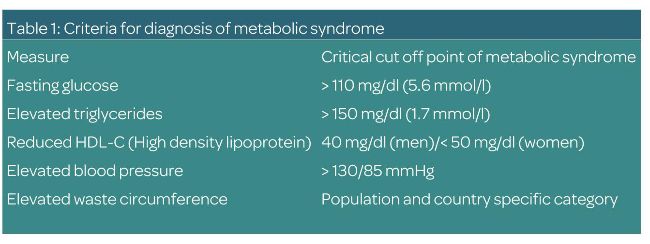
Essentially, the NHS defines metabolic syndrome as a combination of diabetes, high blood pressure and obesity. It puts people at greater risk of coronary heart disease, stroke and other conditions that affect the blood vessels.4(see Table 1)
THE PATHOPHYSIOLOGY OF METABOLIC SYNDROME
Metabolic syndrome is not an isolated disease, but an evolving process trigged by visceral obesity, underpinned by insulin resistance and chronic inflammation.5
Insulin resistance is defined as the reduced responsiveness of target tissues to normal insulin levels, which forms the basis of the pathophysiology of metabolic syndrome.6
Visceral obesity increases the amount of free fatty acids, leading to a reduced uptake of glucose in the muscles. Whilst in the liver, the free fatty acids increase the production of glucose by gluconeogenesis, leading to an increase insulin secretion from the pancreas where insulin also possess lipolytic effects. This results in a further increase of free fatty acids, thereby perpetuating the cycle.7
Metabolic syndrome is not an isolated disease but an evolving process trigged by visceral obesity
In addition, the free fatty acids also increase triglyceride and very low-density lipoprotein (VLDL) production in the liver, whilst decreasing the level of high-density lipoproteins (HDL). 5
It is therefore important to note that visceral fat cannot be regarded as an inert substance, but rather should be viewed as an endocrine organ where adipocytes are active cells with biochemical functions secreting cytokines. These are active proteins known as adipokines with either pro or antiinflammatory properties.7
Anti-inflammatory adipokines include interleukin-10 (IL-10) interleukin- 4(IL-4), adiponectin, secreted frizzle related protein 5 (SFRP5) and omentin-1, while proinflammatory adipokines include interleukin-6 (IL-6) and interleukin-1
(IL-1) tumour necrosis factor alpha (TNF-a).5
An increased level of pro-inflammatory cytokines leads to a continuous low-grade inflammation, especially with individuals impacted by metabolic syndrome.
THE PREVALENCE OF METABOLIC SYNDROME
Over the last decade, there has been an overwhelming increase in the prevalence of metabolic syndrome. According to research, almost a third of the global population are significantly affected; impacting on both morbidity and mortality.7
Changes in dietary habits with higher calorie intake and a sedentary lifestyle are thought to be the two contributors in the rise of the obesity levels. In essence, metabolic syndrome is seen as a global epidemic impacting on quality of life from both a health and cost rspective.3
The link between metabolic syndrome and the skin seems to involve three elements comprising inflammation, oxidative stress and endocrine abnormalities.2
Adipocyte originated leptin tumour necrosis factor (TNF-), interleukin-6 (IL)-6, IL-4, and monocycle chemotactic protein 1 play an important role in the pathology of insulin resistance and certain skin disorders.8
The function of the skin is to provide both a mechanical and chemical barrier.
The mechanical is the barrier between the body and the surrounding environment, whereas, the chemical barrier is medicated by three systems.9These are:
• Reactive oxygen species scavenging system
• Xenobiotic bio-transformation system
• Sebum/sweat excretory system
Oxidative stress is defined as an imbalance between the oxidants and the antioxidants, resulting in the amount of reactive oxygen species (ROS) to be higher than the antioxidant capacity in the body.
Therefore, an excess of ROS may result in lipid peroxidation, oxidative DNA damage and protein oxidation.2
The major sources of ROS are components known as xenobiotics.
These include exogenous chemicals such as drugs, environmental pollutants, cosmetics, and dietary components, which may be eliminated through the skin.9
In addition, the skin expresses xenobiotic metabolising enzymes including cytochrome P450, flavin-dependent mono-oxygenase, monoamine oxidase, alcohol dehydrogenase, aldehyde dehydrogenase and glutathione S-transferase.2
There has been an increased interest in the role of the microbiome and its relationship with inflammation and metabolism.
Observational human studies have shown gut microbial diversity in lean and obese subjects, as well as those with different diet composition.10
Similar differences in microbiota composition were also observed in those with and without type II diabetes mellitus.11
What’s also interesting is that some studies have demonstrated that infusion of microbiota via gastrointestinal probe has alterations in insulin sensitivity.12
Check out next month’s issue for an overview on the skin conditions resulting from metabolic syndrome and what you can do to help.
REFERENCES
1. Hjermann I. (1992). The metabolic cardiovascular syndrome: syndrome X, Reaven’s syndrome, insulin resistance syndrome, atherothrombogenic syndrome. Journal of cardiovascular pharmacology, 20 Suppl 8, S5–S10. https://doi.org/10.1097/00005344-199200208- 00002. 2. Padhi, T. and Garima, 2013. Metabolic syndrome and skin: Psoriasis and beyond. Indian Journal of Dermatology, [online] 58(4), p.299. Available at: <https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC3726879/> [Accessed 7 April 2022]. 3. Lam, D. and LeRoith, D., 2019. Metabolic Syndrome. [online] Ncbi.nlm.nih.gov. Available at: <http://www.ncbi.nlm.nih.gov/books/
NBK278936/> [Accessed 7 April 2022]. 4. NHS, Metabolic Syndrome <https://www.nhs. uk/conditions/metabolic-syndrome/> 5. Lian, N. and Chen, M., 2019. Metabolic Syndrome and Skin Disease: Potential Connection and Risk. International Journal of Dermatology and Venereology, 2(2), pp.89-93. 6. Zhou, S., Li, D., Zhou, Y. and Cao, J., 2012.
The skin function: a factor of anti-metabolic syndrome. Diabetology & Metabolic Syndrome, 4(1). 7. Fatima, F., Das, A., Kumar, P. and Datta, D., 2021.
Skin and metabolic syndrome: An evidence based comprehensive review. [online] E-ijd.org. Available at: <https://www.e-ijd.org/article.asp?issn=0019- 5154;year=2021;volume=66;issue=3;spage=30 2;epage=307;aulast=Fatima> [Accessed 7 April 2022]. 8. Adibi, N. and Robati, R., 2021. Skin and metabolic syndrome: A review of the possible associations.
Journal of Research in Medical Sciences, 26(1), p.16. 9. Zhou, S., Li, D., Zhou, Y. and Cao, J., 2012.
The skin function: a factor of anti-metabolic syndrome. Diabetology & Metabolic Syndrome, 4(1). 10. De Filippo, C., Cavalieri, D., Di Paola, M., Ramazzotti, M., Poullet, J., Massart, S., Collini, S., Pieraccini, G. and Lionetti, P., 2010. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proceedings of the National Academy of Sciences, 107(33), pp.14691-14696. 11. Larsen, N., Vogensen, F., van den Berg, F., Nielsen, D., Andreasen, A., Pedersen, B., Al-Soud, W., Sørensen, S., Hansen, L. and Jakobsen, M., 2010. Gut Microbiota in Human Adults with Type 2
Diabetes Differs from Non-Diabetic Adults. PLoS ONE, 5(2), p.e9085. 12. Vrieze, A., Van Nood, E., Holleman, F., Salojärvi, J., Kootte, R., Bartelsman, J., Dallinga–Thie, G., Ackermans, M., Serlie, M., Oozeer, R., Derrien, M., Druesne, A., Van Hylckama Vlieg, J., Bloks, V., Groen, A., Heilig, H., Zoetendal, E., Stroes, E., de Vos, W., Hoekstra, J. and Nieuwdorp, M., 2012.
Transfer of Intestinal Microbiota From Lean Donors Increases Insulin Sensitivity in Individuals With Metabolic Syndrome. Gastroenterology, 143(4), pp.913-916.e7.

BALSAM ALABASSI
Balsam Alabassi is the founder of DermRefine Skin Clinic, Mayfair, London. She is an independent prescriber and an advanced skin specialist with a Level 7 qualification in cosmetic injectables as well an NVQ Level 4 in laser hair removal and advanced skin rejuvenation. With over 20 years of clinical pharmacy and leadership experience, her mission is to educate, enable and empower her patients to truly own their skin and skin health.